Abstract
Introduction
A significant challenge in the aging hemophilia population is cardiovascular disease (CVD). It is relevant to study cardiometabolic risk factors in children, because the origins of CVD begin in childhood. Risk factors include obesity, hypertension, abnormal lipid profile, and family history of CVD. The prevalence of cardiometabolic risk factors in children with hemophilia is unknown. The objective of this study was to quantify these risk factors and to evaluate the impact of overweight/obesity on target joints and factor consumption.
Methods
Males, 5-20y old, with congenital hemophilia A or B, were enrolled in a cross-sectional study at Rady Children's Hospital San Diego Hemophilia Treatment Center (HTC). Study procedures included standardized measurement of weight, height, waist circumference and blood pressure (BP), and non-fasting laboratory measurement of glucose (<200 mg/dL is normal) and lipid panel (to calculate non-high-density lipoprotein [non-HDL-C]; result was categorized as normal, borderline high, or high per age-based norms). Body mass index (BMI) percentile was determined for children <18 years, and BMI was calculated for adults. Weight category of underweight, normal weight, overweight or obese was assigned based on established norms for BMI percentile and BMI. Waist:height ratio (WHtR) was calculated; >0.5 is considered a cardiometabolic risk factor. (Pre) hypertension was defined as systolic BP (SBP) and/or diastolic BP (DBP) ≥90% for children <18y and SBP >140 or DBP >90 for adults. Parents and adult patients completed questionnaires regarding demographics, personal and family history of CVD, and physical activity. Clinical data were abstracted from the medical record. Descriptive statistics were used to characterize the population. Student's t-test, correlation and chi square test were performed to analyze the data.
Results
Forty-three males (mean 12y, range 5-20y, including 6 young adults) were enrolled. The majority were White race (88%) and Hispanic ethnicity (65%). Twenty-three (53.5%) had severe hemophilia A including 2 with high titer inhibitors.
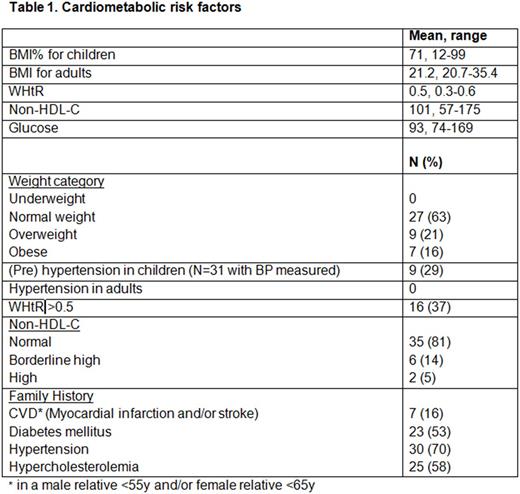
No subjects reported congenital heart disease, kidney disease, diabetes mellitus, glucose intolerance, hypercholesterolemia, (pre) hypertension, or cardiovascular events. Two subjects reported a diagnosis of overweight/obesity, and both were referred to a weight and wellness program. A summary of cardiometabolic risk factors is shown in Table 1. Subjects with normal weight had more days of >60 minutes of physical activity compared to those with overweight/obesity (5.2 ± 2.4d v. 3.8 ± 2.5d; p=0.07).
Thirty-one (72%) were on continuous prophylaxis including all 21 subjects with severe hemophilia A without inhibitor. The mean prophylactic factor dose in units (IU)/kg/week was 118 IU, range 64 -187. There was no difference between subjects with normal weight (125 IU/kg/week, range 71-187) and subjects with overweight /obesity (111 IU/kg/week, range 64-174); p=0.26, but higher weight was correlated with higher total factor consumption (cor=0.84; p <0.001), up to 12,000 IU per week. There was no difference in history of target joints based on weight category (30% in normal weight v. 25% in overweight/obese, χ2= 0.11, p=0.74).
Conclusions
A high proportion of subjects had modifiable risk factors for CVD which were not previously recognized by the patient or parent. Longitudinal follow-up is warranted to define the natural history of CVD in this population. The HTC team, including a genetic counselor, physical therapist and dietician, can identify risk factors for CVD and develop interventions to target cardiovascular risk reduction. Increasing days of physical activity may lead to decreased overweight/obesity, improved outcomes, and less factor consumption.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal